In the Improve Phase is when the team finally visited TMH and observed the process. Some connecting processes were more thoroughly defined during these observations. For further understanding, the floor layout is shown in Figure 12. The blue outline shows the waiting area and the check-in desk for labs, the physician unit, and the infusion unit. The purple outline shows the physician unit, and the green outline shows the infusion unit. Finally, the pink outline shows the pharmacy area where the medication is prepped. The numbers on the figure adhere to the following numbered list which explains the movement of the patient.
1.The patient enters the are through the elevators or stairs.
2.The patient checks in at the lab check-in then waits.
3.Patient gets lab work done.
4.Patient checks in at the physician check-in and waits.
5.Patient is placed in an exam room to see the physician.
6.Patient checks out at physician check-out.
7.Patient checks-in at infusion check-in and waits.
8.Patient is escorted to an infusion chair in the infusion unit and receives treatment. Patient checks-out with the nurse while at the infusion chair.
9.Patient leaves through the elevators or stairs.
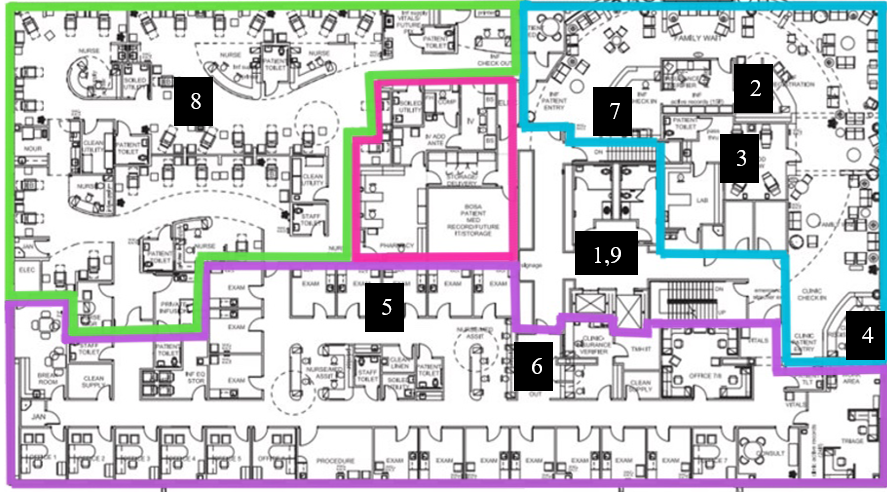
Figure 12: Patient Movement Through Cancer Center
Through observations and data analyis, the root causes of low infusion chair utilization are determined to be the lab capacity and the preset appointment time lengths. The lab space only contains four lab chairs and there are five pods which hold six infusion chairs each. The lab capacity constraint adds to the bottleneck seen during peak hours of 10AM – 3 PM. It would be in the best interest for TMH to add more lab chairs and corresponding machines to process blood work. Adding more chairs without adding more machines will continue to create a bottleneck in the lab. The set appointment lengths were guessed by TMH management when first opened and the appointment lengths have not been revised since. This is why there are so many appointment defects seen during the measurement and analysis of the data. Revising the appointment lengths would allow for better utilization of infusion chair time. With this improvement, TMH could also treat more patients in a day because the data analysis showed infusion appointments running under schedule. This is especially seen for Chemotherapy which makes up for 60.5% of all infusion appointments in 2019.
The team is also suggesting some other improvements which will eliminate time and movement wastes. The check-in area has three check-in desks and this can become confusing for the patient when there is no clear signage. Currently, there is only a sheet of paper taped to a safety glass at each sign-in. Upon entering the Cancer Center, patients habitually go to the first sign-in desk seen which is the infusion check-in. The infusion check-in is the very last check-in during the process so patients usually have to be directed elsewhere. This causes for excess patient movement and time lost for both the patient and check-in technicians. Eliminating this waste will create more time for patients to be seen. Secondly, there are opaque cabinet doors in the infusion pods as seen in Figure 13. Within these cabinets are bins, numbered by infusion chair, to hold the chemotherapy (yellow bin) or medicine (white bin) once they have been brought over by the pharmacy. The nurses consistently peer inside the cabinets to see if their infusion has been dropped off. To eliminate this waste, the team is suggesting to switch out the opaque doors for transparent ones.

Figure 13: Opaque Cabinets Containing Infusions
• Consultation: A consultation will be had with the pharmacy manager, nurse manager, and team sponsor, in which the team will receive feedback on specific proposed improvements. The team will seek approval from the pharmacy's current manager for scheduling implementations. The nurse manager will have valuable insight on improving signage and other operations affected by suggested changes. This will allow for decision making to be more informed and likely increase the satisfaction from stakeholders.
• Proof of Concept: The team will develop a presentation to demonstrate the feasibility of the proposed methods. Notable measurements will be discussed to verify the practical potential of the implementations.
• Solution Assignments: The solutions will be broken down with concise methods of implementation, in which concise methods of implementation will be identified. With the content of this presentation, managerial staff will have sufficient information to determine which staff should execute the proposed solutions.
• Implementations: With the help of Team 403, the final solutions, approved by stakeholders and presented to managerial staff, will be executed. The team will validate the accuracy and monitor the implementations to ensure that the execution aligns with solution parameters, backed by previous data analysis.